Clarifying various Aspects of Health Care Delivery
American readers:
Many of us here in Canada think that your leader, President Obama, is
clear-eyed and wise and is trying to guide you to a crucial choice. Please heed
him. Good luck and good health. This article looks at, and tries to clarify,
centralization and decentralization, rural + regional + medical school delivery
spectra, free enterprise versus socialism, & other currently controversial
and ever-relevant health care topics. Caution: this is 'merely' one old
Canadian doctor's perspective on some internal aspects of universal medicare.
Nevertheless please think on it.
CENTRALIZATION
VERSUS DECENTRALIZATION OF HEALTH CARE
SPECIALISTS VS
GENERALISTS, NURSES VS DOCTORS, SCIENCE VS ART
COMPASSION VS
COMPETENCE, HUNCH VS EVIDENCE...
A FALSE DICHOTOMY in Aspects of Health Care Delivery?
The blind leading the blind by Bruegel. Where is your country? Your leader?
Our country, Canada, unlike the United States, is certainly not in the category of Bruegel's medieval depiction of life-disabled. We have a fair to middling Medicare. It's flawed, but still working. Our life expectancy is high. Our perinatal death rate low. Our people are getting taller and stronger (perhaps not always slimmer). But, some of our leaders are blind, if not stupid, and are on the verge of bogging us all down as in the picture above.
One factor to
consider in looking at health care is this: Is there a trend to
periodic or cyclical change in health care per se and its delivery? Yes. Over
the years, there have been periodic swings in ideas about where to place
medical services. Right now (2009), for instance, the Niagara Health System
(NHS in Canada) is shrinking away from its more outlying areas in order to
concentrate services centrally. Fifty years ago, on the other hand, before NHS
was ever thought of, there was a strong movement to locate numbers of medical
services outward, to wherever people lived. Before that, at the turn of the
twentieth century, the American-generated Flexner Report focused upon upgrading
the quality of medical education, and hence medical practice, all over North
America – effecting a dramatic and seminal historical shift away from the horse
and buggy doctor. So there are always changes afoot, sometimes rational,
sometimes fashionable.
Each of these
changes was accompanied by its own rationale, sometimes reaching an irrational
level of propaganda. Certainly there was – and is – hype by whatever name.
These movements or ideologies cannot be all right or all wrong, as their proponents
and opponents would have us believe. So, where lies the truth?
It is noteworthy that, more or less coincidental to
the above changes, the idea of universal health care, or medicine for the
masses, began to be thought about and in some places applied. What has driven
it is the inevitable advancement of human rights in general. Not economics. Not
politics. Not medical science. Medicare for all is a branch of the Human Rights
Movement. Consider it a special basic human right! The other three changes
noted above – better doctors, local access, specialization centrally – have
been driven by entirely different ideologies or motives.
How does the
healthcare delivery system work?
What is
meant by health care delivery system?
What are
the different types of healthcare delivery systems?
What are the four basic components of all healthcare delivery systems?
What are
the types of healthcare delivery systems?
What is
health care delivery system in USA?
What are the 2 main objectives of a health delivery system?
What is the
health care delivery system?
Why did you
choose to work in healthcare?
What are the four function of health care delivery?
SCIENCE & better doctors
A hundred years
ago, to the Art of doctoring was added science. Science became the driving force
in all of medicine. Flexner, a non-medical teacher and renowned scholar,
essentially said, expose young MDs in training to the discoveries of Pasteur,
Lister, etc., and the practises of such as Osler, and you will all have more
competent doctors. It could only be hoped that compassion was not lost in the
process.
SPECIALIZATION
centrally
Now, it being said
that scientific medicine is preferable to quackery, we can take an honest look
at the seemingly mutually exclusive delivery systems involved in decentralization
and centralization and other seemingly mutually exclusive ways and means.
First, however, it should be said that one particular type of doctor – the
general practitioner or family doctor – never took part in either of those
delivery-shifting movements. That species of doctor, however demeaned or
lionized, whether doing house calls or not, has always been where the people
are – not merely in small towns and the rural countryside, but also in the big
cities and even at the universities – everywhere. I am not saying this to extol
the virtues of the family GP. It's to point out that the issue of
centralization over decentralization has been the domain of the specialist and
never the generalist. The specialization of medicine, and its interpretation and
implementation by managers, has somehow played a major part in and determined
the prevailing fashion of 'sophisticated' service delivery. I must also point
out that the interpretation by managers and bureaucrats sometimes can be driven
by other factors besides the science of medicine. Economics, power-grabbing, or
even fraud, often are disguised by an impassioned public appeal to the 'wise
use' of resources. Catch-phrases crop up: 'best practise' or 'modern medical
methodology' or 'centres of excellence' or whatever appellation can best get
across what is wanted to be gotten across by those who know how to spin things.
Two types of leadership: I'll boil it down to another
most important underlying factor, right here, in two sentences: 1) When doctors
(instead of managers) run medicine, doctors and services tend to go where the
people are at. Good! But the specialist doctors, being closet prima-donnas,
always like to play the leading role. Even in the midst of complaining, they
enjoy running big specialized hospitals at the very centre of things. They'd
even take over the smaller peripheral hospitals if the country doctors would
let them. (Now don't get me wrong, I'm a specialist, a super-specialist, a
former med school teacher – and I like specialists. But I've also always done
general medical practice. So I think I understand how things stand with all the
different brands of my fellow doctors.) Now I'll get tough. 2) When managers
run medicine, they want all the specialists in one spot, the family doctors be
damned. For they often see non-specialists (in their lingo) as no better
equipped than nurses and certainly not as good as paramedics. (In some cases
they might be right.) The managers then claim that big centralized, specialized
hospitals are best for all. Peripheral places are useless. So, total managed
medicine is like the cart pulling the horse. You must be wondering, is there
any rationality in any of this? Well, not unless you really go a step further
and break it all down into a very simple question and that is: What works best?
Let's proceed by
breaking that crucial question down at three clear levels: what works in 1)
outlying areas, 2) regional centres, and 3) schools of medicine (nursing,
paramedical, lab support, etc.). We'll look briefly at each, starting with the
last.
The university centre: Medical schools have to have
the departments you should never see elsewhere. That would include reproductive
science, genetic research, anatomy, physiology, heart and lung transplants and
the like. I also think that Schedule A (tertiary) Psychiatric Hospitals should
be university hospitals. But, to get on with my point, as the med schools have
student doctors to teach, they also must have a bit of everything else, the
mundane clinical things, quite readily on tap. Granted! But they'll never have
rural medicine in a university town, so, if they want to produce any
well-versed doctors of that sort, they must rotate them out to the boondocks
for locum tenems on the hoof. As a case in point, when I taught at the
University of Buffalo's medical school, I sent/brought family practice
residents across the border to work and learn in small-town (Fort Erie) and
small-city (Welland) emergency departments. They taught us too! That's all I'll
say about that, as it is just background to our main concerns, regional and
outlying areas.
The wider region: An axiom of the foregoing (limits
ascribed to academe), is that regions (like Niagara) shouldn't be playing the
game of 'we're as good as any medical school.' They aren't and they cant be.
But they can be topflight (up to a point) clinically. Any goodly-sized region
should have a centralized burn and trauma centre, a state of the art cancer
treatment service, a child psychiatry centre of excellence, a ... the list
should be worked out by the specialists in consultation with family doctors
and, believe it or not, by getting feedback from the 'raw material' of it all –
patients, people at large, politicians (a bit), economists, and whoever else
might have some kind of relevant stake in it. (But don't be overwhelmed. When
in the Soo-Algoma region, I was swamped with the personal, idiosyncratic
suggestions of too many people altogether. This person said addiction came
first, that person said, catch them young - children come first. Not being a
Solomon, I decided to set up a community register that reflected what was
really needed as opposed to what was merely wanted. What came highest were
services for the indigenous peoples. Then I ran into evidence of denial and/or
bigotry. "We do not have those problems here," and the like. Then
came arguments about whose responsibility is it? "Not ours - it belongs to
the Federal government." Eventually, rationally phrased statistics in
concert with public wishes prevailed.) What I'm saying is, don't be
boondoggled, be properly informed. We need to be aware of the actual and the
possible, what is ideal and what is economically feasible. Some
medical-surgical services ought to be very well centralized in a fine regional
hospital. And some things should not. Some services should be recognized as
primary, all across the board. Those services ought to be spread outward and
around.
LOCAL access of Health Care Delivery
Now for a brief
diversion to make the next point, which is - getting things closer to patients:
Back in the 1960s the community mental health movement epitomized
decentralization. It was humane, emptied the hundred year old, monster,
'snake-pit' mental 'asylums' (with a boost from the new anti-psychotic
medications), put psychiatric wards in just about every medium sized general
hospital and – ultimately failed because money was not forthcoming to go a step
further and provide true community care. Sad sick mental patients are seen
lolling on every city's sidewalks, as a result. But even this failed social experiment,
hyped as modern science, was not entirely rational. Founded upon President
Kennedy's personal concern for people like his intellectually retarded sister
(only somewhat like in actuality), it obviously had a deeper motive. It was a
pet personal project. But as legislation was passed, it was laced with unproven
hypotheses, all given wild political spin. So, a good thing unfinished,
presumed modern, can simply become the fashion of the day or decade.
Outlying places:
The 'specialities' that should not be centralized are primary,
core-medical-skills that are translated into services that belong as close to
every patient's home as possible. They need to be in the medium sized city
hospitals and some even in outlying rural hospitals. What are these core services?
Emergency rooms, diagnostic labs and varying levels of imaging, small
obstetrical units and miniature paediatric wards, low to medium level cardiac
intensive care units, day surgery (not too specialized), some beds for the
treatment of medical illnesses and near-home geriatric and psychiatric care,
and a selection of specialized outpatient departments. As one gets further out
into the periphery, these various core services can and should be manned by
generalists, not specialists. Specialists should be on tap as consultants but
not in primary charge of patients. The family doctor is a natural front line
coordinator and doer and should be on top of what happens to patients. More
specifically, emergency departments in medium sized cities need ER specialists,
but those in small rural hospitals can be handled quite adequately by
experienced and up to date GPs. If an outlying hospital could have nothing
else, that one thing should be an ER. Finally, no emergency room can safely be
more than ten to fifteen minutes away by ambulance from anyone in its catchment
area, else time-critical life or death emergency patients will die in transit.
This crass slogan applies: there will be – deaths - otherwise.
Obviously, I am
touting the much neglected needs of outlying areas here. Why? If small town
people are not catered to every bit as well as those in larger places the human
rights aspect of universal health care is betrayed. But aside from that, it has
been shown that decentralized medicine and hospital care, in small towns and
small cities alike, is not only close to home and hence humane, but also more
cost-effective than super-specialized and over-centralized Medicare.
Innovation: Everyone can reap the benefits of the most sophisticated of
specialities – cheaply! By capitalizing upon local talent, which is indigenous
all over – in rural areas, small towns, medium sized cities – millions of
dollars can be saved. Front line people are capable. Innovation works! In child
psychiatry (more generally too), I once had a choice of creating expensive
central clinics with huge staffs or setting up highly responsive roving
casualty teams that visited the schools, children's aids, the courts, etc. By
so doing, the real front line workers, public health nurses, teachers, very
junior social workers, police juvenile officers, clerics, the list is long,
were educated right on the spot and recruited to help upset children during
crises, on the hoof. This was shown to work in Hamilton, Sault Ste. Marie,
Haldimand-Norfolk, even Wawa. So, no one can ever tell me that the whole answer
is mere bricks and money. It's so easy, costly, and potentially harmful to
'export' patients to a far away 'centre of excellence.' Patient-centred,
flexibility, outsight, innovation, mobility, and respect for indigenous
front-line talent are the key words and ideas.
Dealing with
managers, media, and their ploys: Dichotomous controversies can be the spice of
life – at least the spice of media coverage. Remember, something repeated a
thousand times becomes the 'truth.' Here are 18 common health care propositions
of present day Goebbels-in-disguise. Test yourself:
An apple a day... of Health Care Delivery
Hold on now! I'm
not gonna be confined to any simple-minded, yes or no, answer. And I certainly
will not be confused by multiple questions in one sentence. I have a brain in
my head and must think on it. I'll take time out to ponder the issues. There's
more than one way to skin a cat. Now that's gotta be true. Maybe.
A single note to
physicians: Too many Canadian doctors are altogether too polite and agreeable.
Under that facade, they may actually feel ineffectual. So they come across as
disinterested and apathetic about general health care controversies. They look
to Big Brother in the medical society (CMA, OMA, etc.) to fix things for them.
They may even that government will fix things for their
patients. Not very likely! Not without strong medical input. Anyway, doctors
tend to lay back and wait while Rome burns. But we doctors can do useful things
locally in little ways. Here's just one: We should, of course, be able to agree
to disagree – in abstract philosophical discussions. But, if a lay-manager
implies that you should politely do just that, agree to disagree agreeably,
even though s/he is actively pressing ahead with some medically foolish act or
a totally bureaucratic change, recognize it as a ploy and disagree
vociferously. Here's another piece of advice – to GPs: Don't be squeezed out of
work to become only a paper-pushing referral agent. Keep up your front line generic
skills. Become THE expert on the family. Learn how to do some real counselling
– individual, marital, family. Deliver babies. Above all, take ER call-duty. Do
not let any insurer, manager – or specialist for that matter – reduce you. You
are the basis of all Medicare. Put your foot down and dig in your heels.
Conclusions:
Finally, to reiterate, it's not centralization OR decentralization. It's what and how much where. It is getting core services out to people where they live. It's concentrating highly specialized resources at an accessible central point.
It's not starving or dismantling outlying services supposedly to put up central
bricks. And it's utilizing all doctors, including GPs, at the points in the
delivery system where they'll do most good. I might add that accountants,
managers and government bureaucrats have a crucial role in health care, and
that is helping with money matters and ensuring that medical services are
delivered rationally. Not by whim or by idiosyncratic ideology. Certainly not as
silly power ploys designed to build personal empires. All parties, especially
politicians, big money private sources, and consumers too, must clearly
recognize that medicine or health care delivery is a human service, not a
manufacturer of material goods. In that respect the health field does not
satisfy the usual commercial-business laws of simple supply and demand – need,
or demand, is always outrunning supply. Why? New discoveries perpetually create
ever-expanding demands. So costs, even streamlined, will always go up, and up
... but fact (or hope?) of ordinary people helping people is always the same.
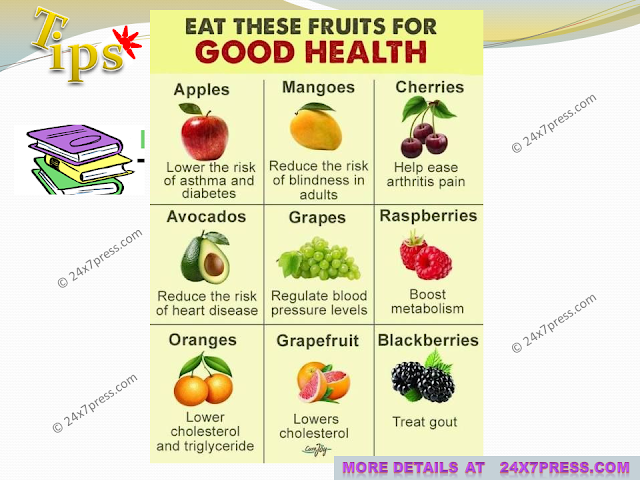
More tips for good heath
What are the four function of health care delivery?
What are the four functions of
health systems?
Progress
towards them depends on how systems carry out four vital functions:
provision of health care services, resource generation,
financing, and stewardship. Other dimensions for the evaluation of health
systems include quality, efficiency, acceptability, and equity.
What are the main objectives
of a health care delivery system?
The primary
objectives of any health delivery system are to
enable all citizens to receive health care services whenever
needed, and to deliver health services that are cost-effective
and meet pre-established standards of quality.
What is a health care delivery
system?
A health
care delivery system is an organization of people, institutions, and
resources to deliver health care services to meet the health needs
of a target population.
What are the four major
services in healthcare?
The four
major services of healthcare are:
Health Promotion.
Disease Prevention.
Diagnosis and Treatment.
Rehabilitation. Health care
provides primary care, secondary care, tertiary care, and public care.
What are the essential
functions of a health system?
Inform,
educate, and empower people about health issues. Mobilize
community partnerships and action to identify and solve health problems.
Develop policies and plans that support individual and community health efforts.
Enforce laws and regulations that protect health and ensure
safety.
What are the major components
of a health care system?
In this
model, adapted from Ferlie and Shortell (2001), the health care system is
divided into four “nested” levels: (1) the individual patient;
(2) the care team, which includes professional care providers
(e.g., clinicians, pharmacists, and others), the patient, and family members;
(3) the organization
What are the types of
healthcare delivery systems?
What You Need to
Know About 4 New Healthcare Delivery Systems
Managed Care.
Managed care plans aren't new, but these plans are continually undergoing
changes due to President Barack Obama's healthcare law. ...
Concierge Services. ...
Self-Directed Services. ...
Telemedicine.
What is the difference between
public health and healthcare?
For
example, public health personnel work within communities,
organizations, and government to direct and enforce public
health policies. On the other hand, healthcare administrators
support the activities of primary care givers in health institutions
such as hospitals, nursing homes, and outpatient centers.
What are the 3 levels of
healthcare?
What are
services in healthcare?
What are
the two types of healthcare services?
What are
the two categories of health care services?
What are the 10 essential health
care benefits?
What are the
four components of public health?
What is
the difference between public health and healthcare?
What makes
a good health care system?
What are the six components of
health?
What is an
ideal healthcare system?
What are
the basic components of the healthcare delivery system?
What is a delivery system What
are some examples?
What role
does public health have in medical care?
What is
the role of public health in the healthcare delivery system?