“Doctor, I have an upset stomach” -- What is “dyspepsia”?
“Doctor, I have pain in the abdomen” -- What is NOT “dyspepsia”?
How common is dyspepsia?
“So I have dyspepsia. What is causing it?”
Two important factors to consider in diseases associated with dyspepsia
Approach to the patient with “uninvestigated dyspepsia”
What about an abdominal ultrasound?
If a cause for dyspepsia is found, what are the treatments?
What is functional dyspepsia?
Dyspepsia and normal endoscopy: Two notes of cautionThe term “dyspepsia”
is used in medical writing, but it is not used in everyday life, and patients
do not come to a doctor saying “I have dyspepsia.” However, it is very common
for people to express that they have “upset stomach,” “indigestion,” “acid
stomach,” “acid indigestion,” “stomach pain,” “stomach burning,” or “stomach
fullness.” These and similar terms reflect the experience of abdominal pain or
discomfort, often worsened by eating. It is also common for people to complain
of “heartburn,” which to some means upper abdominal burning alone, but for many
it consists of a burning sensation in the chest.
A concise definition of dyspepsia is
chronic or recurrent abdominal pain or discomfort in the upper abdomen.[1]
Researchers debate the distinction between “pain” and “discomfort” but most
recognize that some patients with “dyspepsia” do not have pain, yet they are
bothered by other symptoms that can include an uncomfortable sensation in the
upper abdomen, losing appetite after eating very little, and feeling full after
eating.[2] Some patients may also experience nausea, an unpleasant sensation
that they may soon need to vomit. The term “dyspepsia” is used to capture this
group of digestive symptoms, which are believed to arise from the stomach and
upper gut.[3]
It has been controversial whether “heartburn” should be considered separately
from “dyspepsia” or whether it should be part of the “dyspepsia umbrella.” The
practical reason for a distinction is that “heartburn” is more likely than
“dyspepsia” to be explained by acid reflux (passage of stomach acid to the
esophagus, which is the “swallowing tube” in the chest, between the mouth and
stomach). The approach to patients with acid reflux, or gastroesophageal reflux
disease (GERD), differs from the approach to patients with dyspepsia without
prominent “heartburn.” For this reason, recent guidelines recommend that
patients who have heartburn predominantly should be considered initially to
have gastroesophageal reflux disease and should not be grouped with patients
with dyspepsia.[2-4] However, it is recognized that some patients with
“dyspepsia” do actually have gastroesophageal reflux disease without classic
heartburn, and that some without demonstrable gastroesophageal reflux disease
may experience heartburn as one of their symptoms.
“Doctor, I have pain in the abdomen” -- What is NOT “dyspepsia”?
Patients with the variety of symptoms
described above may be said to have “dyspepsia,” but it is important to
recognize patients with other patterns of symptoms that should not be confused
with “dyspepsia.” Acute abdominal pain (pain that comes on suddenly and has not
happened before) is not dyspepsia. Depending on the nature of the pain and
other symptoms, acute abdominal pain may represent medical emergencies such as
serious inflammation of the gallbladder or pancreas, intestinal blockage, loss
of blood flow to the intestines, appendicitis, a gynecological emergency, a
heart attack, or other serious diseases. Severe acute abdominal pain should be
considered an emergency.
Gallstones can lead to recurrent attacks of upper abdominal pain, which may be
severe and may be accompanied by nausea, back or shoulder pain, and sweating.
People may often feel completely fine for weeks between such attacks. This
symptom pattern should be distinguished from the pattern of more frequent –
even daily – and generally milder symptoms that is implied by
“dyspepsia.”
It is common for patients to experience
abdominal pain and changes in their bowel function, such as diarrhea or
constipation. These symptoms may have many causes, including an acute
infection, metabolic problems, inflammatory bowel disease, celiac disease, and
irritable bowel syndrome. This group of persons should be considered separately
from those with dyspepsia.
How common is dyspepsia?
In Western countries, approximately 25% of
people experience dyspepsia in any given year.[1] Many do not see a doctor, and
self-medication is common, as attested to by the many products that are
available over the counter for various digestive symptoms. For most persons
with dyspepsia, it is a chronic problem, although the intensity and frequency
can vary over the years. Approximately 1% of people may develop new dyspepsia
every year, with a similar number becoming free of dyspepsia, so that the
number of people with dyspepsia in the population remains stable.[1] Dyspepsia
is a common reason for a medical visit, accounting for 2-5% of family practice
consultations and a significant number of referrals to gastroenterologists.
“So I have dyspepsia. What is causing it?”
Before discussing how to approach patients
with dyspepsia, including what tests or treatments should be considered, it is
important to understand the possible causes of dyspepsia and how likely they
are. Appreciating these possible causes lays the logical foundation for the
currently recommended approaches to patients with dyspepsia.
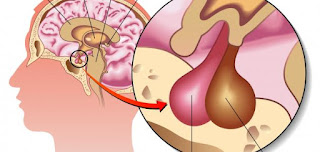
In patients who have endoscopy (a “camera scope” exam of the upper esophagus,
stomach, and upper small intestine, known as the duodenum) to try to determine
the cause of dyspepsia, the types of abnormalities that can be uncovered
include:
- Stomach or
duodenal ulcer
- Gastroesophageal reflux disease with or without visible damage to
the esophagus (esophagitis)
- Stomach cancer, which is the least common underlying disease in
persons with dyspepsia, but fear of which may drive people to see a doctor
- No
abnormality
Patients may find it remarkable, but over half of people with dyspepsia do not
have any identifiable abnormalities on routine medical testing. This group of
people is labeled as having “functional dyspepsia,” also known as “non-ulcer
dyspepsia” or “idiopathic dyspepsia” (“idiopathic” means we do not know what
causes it). Not finding an abnormality can be a source of both relief and
frustration for patients and doctors, and the management of persons with
functional dyspepsia can be challenging, as discussed below.
The likelihood of the various cause of dyspepsia differs between countries and
even between specific locations within countries, and is affected by patient
age and other factors. In North America, it is estimated that peptic ulcer
disease accounts for 5-15% of cases of dyspepsia, gastroesophageal reflux
disease for 15-30%, cancer for less than 1-2%, and functional dyspepsia for
over 50%.[1] Older patients are more likely to have cancer than younger
patients, but even in older patients cancer is an uncommon explanation for
dyspepsia.
Two important factors to consider in diseases associated with dyspepsia
There are two very important factors to
consider when developing management strategies for persons with dyspepsia.
These are aspirin and non-steroidal anti-inflammatory drugs (NSAIDs) such as
ibuprofen (Motrin, Advil) and naproxen (Aleve), and the bacterium Helicobacter
pylori (H. pylori). Both are related in important ways to dyspepsia and its
associated diseases.
Aspirin and NSAIDs may cause dyspepsia without causing ulcers. They may also
cause gastrointestinal damage ranging from minor erosions (small areas of
injury that are too small and superficial to be called an ulcer) to severe
ulceration. Ulcers, in turn, may or may not cause dyspepsia. Serious
complications of ulcers can include bleeding, bowel blockage or perforation,
and sometimes patients do not have dyspepsia before these complications occur.
These relationships between aspirin and NSAIDs and dyspepsia and its associated
diseases highlight why it is important to establish whether dyspeptic patients
are using aspirin and NSAIDs. This includes patients who have not yet had any
testing, “investigated patients” (those who have had endoscopy) with proven
ulcer disease, and also in those with no abnormality on upper endoscopy.
H. pylori is a bacterium that lives in the stomachs of hundreds of
millions of people around the world.[5] It is more common in developing
countries and in Asia, Africa and South America than in Western countries.
There is a clear and strong association between H. pylori and
peptic ulcer disease, H. pylori and stomach cancer, and H.
pylori may also be important in a small proportion of persons with
functional dyspepsia. In persons with ulcer disease due to H. pylori,
cure of the infection almost eliminates the chance of developing an ulcer
again, whereas failure to eradicate H. pylori is associated
with a very high rate of recurrent peptic ulcer disease.[6] The vast majority
of people with H. pylori do not develop ulcer disease or
cancer, but H. pylori causes inflammation and other changes in
the stomach lining that can eventually lead to stomach cancer in a small
fraction of infected persons. These relationships between H.
pylori and dyspepsia and its associated diseases form the basis for
the current recommendations on how to approach persons with dyspepsia.
Approach to the patient with “uninvestigated dyspepsia”
A person with dyspepsia who has not had
medical testing (usually endoscopy) to try to determine a cause has
“uninvestigated dyspepsia.” Many studies have tried to determine the optimal
approach in these patients. Unfortunately, the clinical story alone does not
allow doctors to make an accurate diagnosis without testing. Current recommendations
on how to approach patients with uninvestigated dyspepsia are based on an
appreciation of how common the different possible underlying diseases are, and
on the available research studies.[1-3, 7, 8] Performing endoscopy up-front on
all patients with dyspepsia would be the most direct route to determining a
specific diagnosis, but this is not practical in the primary care setting, and
it is not likely to be a viable strategy because it is too costly.
A reasonable stepwise approach begins with determining if a person complaining
of dyspeptic symptoms is taking aspirin or NSAIDs. If so, and if these
medications can be stopped readily, it is reasonable to stop them and observe
to see if the dyspeptic symptoms go away. If the person has a strong reason to
take low-dose aspirin, such as prevention of heart attack or stroke, or to take
NSAIDs, such as treatment of arthritis pain that does not respond to
acetaminophen (Tylenol), a reasonable approach is to take a proton pump
inhibitor along with the aspirin or NSAID. Proton pump inhibitors are
medications that decrease the amount of acid produced by the stomach, and these
medications can improve the dyspepsia associated with aspirin or NSAIDs, as
well as heal or prevent ulcers. The available proton pump inhibitors include
omeprazole (Prilosec, now also available in the United States without
prescription as Prilosec OTC), lansoprazole (Prevacid), rabeprazole (AcipHex),
pantoprazole (Protonix) and esomeprazole (Nexium). It is advisable to take the
lowest possible dose of aspirin and NSAIDs and to use these for the shortest
possible time.
Older persons have a higher risk of cancer than younger persons, and for this
reason guidelines recommend that older persons presenting with dyspepsia should
undergo prompt endoscopy. The precise age cut-off is debated and depends on how
likely cancer is in a given region and on the availability of health services,
but prompt endoscopy is sensible in persons older than 45-55 years of age
presenting with dyspepsia.[1-3]
Most persons with cancer of the upper digestive system have “alarm symptoms”
such as difficulty swallowing, nausea and vomiting, weight loss, vomiting
blood, or black stools (reflecting internal bleeding). Unfortunately, the
presence of alarm symptoms does not seem to be very useful in identifying
persons with cancer versus those without cancer.[9] Nonetheless, most experts
agree that patients with dyspepsia and alarm symptoms should undergo prompt
endoscopy.[2-4]
In younger persons (under 45-55 years of age) without alarm symptoms, the H.
pylori “test-and-treat” strategy is recommended.[2-5, 8] These persons
are unlikely to have cancer, a minority may have peptic ulcer disease or
gastroesophageal reflux disease, and most would have a normal upper endoscopy.
In the absence of aspirin or NSAID use, peptic ulcer disease would likely be
due to H. pylori. Treatment of H. pylori can
have several benefits:
- It treats peptic ulcer disease and nearly eliminates the risk of
recurrent ulcer.[6]
- When H. pylori was first discovered, it was hoped
that treating it might cure most persons with dyspepsia but without an
ulcer. Unfortunately, this is not the case, but a small minority of these
patients does seem to benefit. It is estimated that 10-25 persons with
functional dyspepsia and H. pylori need to be treated in
order to cure one.[10]
- It has the potential to decrease the risk of developing ulcers or
stomach cancer later in life.
The currently recommended tests for H. pylori are a stool test
(stool antigen test) or a breath test (urea breath test). If a test for H.
pylori is positive, the recommended first-line treatment is triple
therapy with a proton pump inhibitor combined with amoxicillin 1 gram, and
clarithromycin 500 mg or metronidazole 500 mg, all taken twice a day for 10-14
days.[5] It is important to complete the entire treatment course as prescribed
in order to increase the likelihood that H. pylori will be
eradicated.
If H. pylori is very rare in a particular region, it may be
most cost-effective to offer young persons with dyspepsia without alarm
symptoms a trial of proton pump inhibitor treatment once a day for 4-8 weeks
and then reassess. However, eradicating H. pylori could
decrease future ulcer and cancer risk, and this opportunity is lost when a
proton pump inhibitor trial is given instead of testing for H. pylori.
In Western countries, most patients with dyspepsia will test negative for H.
pylori, leaving the question of how to manage this majority of patients. A
trial of proton pump inhibitor treatment once a day for 4-8 weeks is
recommended for several reasons:
- Gastroesophageal reflux disease is reasonably likely, and proton
pump inhibitors are excellent treatment for this condition.
- Symptoms in functional dyspepsia may improve with proton pump inhibitor
treatment.[11]
- Although ulcers are rare in the absence of H. pylori,
aspirin, or NSAIDs, most ulcers heal with proton pump inhibitor treatment.
Regardless of what initial approach is followed, a substantial number of
persons with dyspepsia will not feel better with the initial treatment or will
experience a return of their symptoms. The options at this point are to re-test
those who had eradication therapy for H. pylori and treat
again with a different regimen if infection persists, to switch from H.
pylori “test-and-treat” to proton pump inhibitor therapy or vice
versa, or to move on to endoscopy. Ultimately, it is reasonable to perform
endoscopy in persons who fail to improve after two attempts at therapy.
Although it is unlikely that endoscopy will uncover any serious abnormality at
this point, it is important to exclude cancer and it is possible that the
reassurance from a normal endoscopy may help decrease the anxiety over possible
serious disease. At the time of endoscopy, stomach biopsy should be performed,
and H. pylori should be treated if it is found on biopsy.
What about an abdominal ultrasound?
Abdominal ultrasound is unlikely to be
useful in patients with dyspepsia. As discussed above, it is important to
distinguish patients who may have pain from gallstones from those with
dyspepsia. Most people with gallstones do not have symptoms from them, and do
not need to have their gallbladder removed. The problem with looking for
gallstones in people with dyspepsia is that they may have gallstones by chance
alone. Removal of the gallbladder in these patients will not help and carries a
small but real risk of complications.
If a cause for dyspepsia is found, what are the treatments?
If endoscopy identifies an explanation for
dyspepsia, then directed management will be possible. Stomach cancer can be
treated depending on the type and extent. Gastroesophageal reflux disease can
be treated with acid suppression. The most potent acid-suppressing medications
are the proton pump inhibitors. Some patients with gastroesophageal reflux
disease may do well with the less potent histamine receptor antagonists such as
cimetidine (Tagamet), ranitidine (Zantac), nizatidine (Axid), or famotidine
(Pepcid), but proton pump inhibitors are usually needed in those with
esophagitis. Gastroesophageal reflux disease often requires long-term, ongoing
treatment. Peptic ulcer disease can be managed by eradicating H.
pylori and avoiding aspirin and NSAIDs. If aspirin or NSAIDs must be
continued, treatment with a proton pump inhibitor will decrease but not
eliminate the risk of ulcer recurrence.
The majority of patients with dyspepsia do
not have an identifiable abnormality at endoscopy, and they are diagnosed with
functional dyspepsia. Functional dyspepsia is one of the common “functional
gastrointestinal disorders,” which are conditions in which patients have
symptoms but standard medical testing is normal.[3] Beginning in the 1980’s,
leading researchers in the field of functional gastrointestinal disorders have
engaged in the “Rome process” (named after the city where the major meetings
for this group have taken place), which addresses multiple issues related to
the study of the functional gastrointestinal disorders. A major task of the Rome
process is to define symptom-based diagnostic criteria for these
disorders.
The Rome III pragmatic definition of functional dyspepsia, proposed in 2006, is
“the presence of symptoms thought to originate in the gastroduodenal region, in
the absence of any organic, systemic, or metabolic disease that is likely to
explain the symptoms.”[3] The Rome III diagnostic criteria for functional
dyspepsia are:[3]
1. One or more of:
a. Bothersome
postprandial (after eating) fullness
b. Early satiation
(early loss of appetite during a meal)
c. Epigastric
(mid-upper abdominal) pain
d. Epigastric burning
AND
2. No evidence of structural disease (including at upper endoscopy) that is
likely to explain the symptoms
* Criteria fulfilled for the last three months with symptom onset at least six
months before diagnosis
The Rome working group has proposed two distinct syndromes under functional
dyspepsia based on the belief that patients described by the two syndromes may
have different underlying abnormalities. These are the “Epigastric Pain
Syndrome,” which is characterized by pain or burning in the upper abdomen, and
the “Postprandial Distress Syndrome,” which is characterized by bothersome
fullness after a meal and/or early loss of appetite that prevents finishing a
regular meal.
Dyspepsia and normal endoscopy: Two notes of caution
Although most patients with dyspepsia and
normal endoscopy are categorized appropriately as having functional dyspepsia,
two notes of caution are needed. First, it is possible for patients to have
gastroesophageal reflux without visible esophagitis, and those with typical
heartburn and regurgitation (passage of stomach contents to the mouth) should
be considered to have gastroesophageal reflux disease and should be treated
with acid suppression. Second, many patients are treated with proton pump
inhibitors before endoscopy, and a small number of them may have had
esophagitis or ulcers when they were initially treated. With treatment,
esophagitis and ulcers can heal and endoscopy can then be normal. If an ulcer
was the cause of pain and the ulcer has healed, one would expect the pain to go
away. If the pain persists, that patient may have ulcer disease as well as
functional dyspepsia.
What causes functional dyspepsia?
Functional dyspepsia is an umbrella term
for what are likely to be a group of different underlying abnormalities. By
definition, standard medical tests do not show abnormalities in functional
dyspepsia, but multiple studies have shown that subgroups of patients with
functional dyspepsia exhibit differences from persons without functional
dyspepsia when specialized tests or research studies are performed.[1, 12]
These include abnormally slow emptying of food from the stomach and other
abnormalities in the motor function of the stomach such as inadequate
relaxation to accept a meal or weak contractions. Subgroups of patients with
functional dyspepsia display “hypersensitivity” to a variety of challenges
including distension of the stomach with a balloon, acid infusion into the
duodenum, or delivery of fat into the intestine. The link between these
abnormalities and patients’ symptoms is not clearly established.
It has been disappointing that in most persons with functional dyspepsia
and H. pylori infection, treatment of the infection does not
cure the dyspepsia. However, there is evidence that a small minority of these
persons do experience cure of their symptoms when H. pylori is
eradicated.[10] There is an association between functional dyspepsia and
psychological factors, including anxiety.
Can all persons with functional dyspepsia really be lumped together in one
group? If they don’t all have the same symptoms, do they all have one
“disorder”? Are there different causes for symptoms in different patients? A
major challenge has been that specific symptoms and specific physiological
“abnormalities” do not go hand in hand. Past attempts to divide people into
those with “ulcer-like” symptoms such as burning pain and those with symptoms
of “dysmotility” (abnormal muscle function of the gastrointestinal tract) such
as fullness or early loss of appetite have not been very successful because of
the significant overlap between groups. It remains to be seen whether the
“Epigastric Pain Syndrome” and “Postprandial Distress Syndrome” will prove to
be useful categories.
Sub-categorization of patients would be most useful if symptoms and/or specific
tests could identify groups that should receive different treatments.
Unfortunately, few treatments are available currently and most tests are
imperfect or impractical.
How is functional dyspepsia managed?
It is disappointing, but the reality is
that the treatment options for functional dyspepsia are limited. Some patients
may do well with education and reassurance. Even though symptoms tend to be
chronic, allaying the fear over serious disease may allow some patients to
adjust and live with their symptoms. No specific dietary advice is universally
successful, and patients should be encouraged to eat a normal, healthy diet.
Limiting fat intake may help some patients.
Many patients wish to try medications to decrease their symptoms and improve
their quality of life. Acid suppression with proton pump inhibitors or
histamine receptor antagonists may help some patients.[11] This may be due to
the fact that some patients who are labeled as having functional dyspepsia
actually have reflux, and that some others may have hypersensitivity to acid in
the stomach or duodenum. Antacids do not seem to be effective.[11] Medications
to improve the motor function of the stomach are limited, some are no longer
available, and it is not clear that available drugs help in functional
dyspepsia.[11]
Patients who have H. pylori should have treatment to eradicate
the infection.[5] It is estimated that 10-25 persons need to be treated to
achieve one cure in functional dyspepsia.[10] Given that there are few
treatment options for functional dyspepsia, these are actually reasonable odds
of success. Eradicating H. pylori may have the additional
benefit of decreasing subsequent risk of ulcer disease and cancer.
Antidepressant medications may help in functional dyspepsia even when patients
are not depressed, but there has been relatively little research in this area.[1]
These medications may affect the perception of symptoms. There is stronger
evidence that antidepressants help in irritable bowel syndrome, another classic
functional gastrointestinal disorder. Antidepressants are used in functional
dyspepsia in part based on an extension of the evidence in irritable bowel
syndrome. The tricyclic antidepressants include amitriptyline (Elavil),
nortriptyline (Pamelor), imipramine (Tofranil), and desipramine (Norpramin),
and the selective serotonin reuptake inhibitors (SSRIs) include fluoxetine
(Prozac), sertraline (Zoloft), paroxetine (Paxil), citalopram (Celexa) and
fluvoxamine (Luvox). The rationale for using these medicines should be
explained to the patient since the doctor-patient relationship can be damaged
if patients look up information on the prescribed drug, learn it is an
“antidepressant” and question their doctor’s justification for prescribing the
medication.
There is some evidence that functional dyspepsia may improve with a variety of
psychiatric treatments.[13] These include hypnotherapy, cognitive therapy,
relaxation, and psychodynamic-interpersonal therapy. It’s not clear how
long-lasting the benefit may be, and these therapies are not currently
available for most patients.
Dyspepsia is very common. Patients with dyspepsia may be concerned that there is something “seriously wrong inside.” Fortunately, serious disease, including cancer, is a very uncommon explanation for dyspepsia. Older patients and those with “alarm symptoms” should have prompt endoscopy. Younger patients without alarm symptoms can be managed without endoscopy initially, with endoscopy reserved for those with persistent symptoms. Eradication of H. pylori infection treats peptic ulcer disease, can decrease the risk of cancer, and may help a minority of patients with functional dyspepsia. Acid suppression is excellent therapy for gastroesophageal reflux disease and may help in functional dyspepsia. Although it can be challenging to treat functional dyspepsia, patients should be reassured that they are not at higher risk of cancer or other serious disease and that they have a normal life expectancy. A variety of treatments can be tried, and the focus should be on leading a normal life even if symptoms cannot be eliminated.
References
1. Talley
NJ, Vakil NB, Moayyedi P. American gastroenterological association technical
review on the evaluation of dyspepsia. Gastroenterology 2005;129:1756-80.
2. Talley
NJ, Vakil N. Guidelines for the management of dyspepsia. Am J Gastroenterol
2005;100:2324-37.
3. Tack
J, Talley NJ, Camilleri M, Holtmann G, Hu P, Malagelada JR, Stanghellini V.
Functional gastroduodenal disorders. Gastroenterology 2006;130:1466-79.
4. Talley
NJ. American Gastroenterological Association medical position statement:
evaluation of dyspepsia. Gastroenterology 2005;129:1753-5.
5. Malfertheiner
P, Megraud F, O'Morain C, Bazzoli F, El-Omar E, Graham D, Hunt R, Rokkas T,
Vakil N, Kuipers EJ. Current concepts in the management of Helicobacter pylori
infection: the Maastricht III Consensus Report. Gut 2007;56:772-81.
6. Ford
AC, Delaney BC, Forman D, Moayyedi P. Eradication therapy for peptic ulcer
disease in Helicobacter pylori positive patients. Cochrane Database Syst Rev
2006:CD003840.
7. Delaney
B, Ford AC, Forman D, Moayyedi P, Qume M. Initial management strategies for
dyspepsia. Cochrane Database Syst Rev 2005:CD001961.
8. Ford
AC, Qume M, Moayyedi P, Arents NL, Lassen AT, Logan RF, McColl KE, Myres P,
Delaney BC. Helicobacter pylori "test and treat" or endoscopy for
managing dyspepsia: an individual patient data meta-analysis. Gastroenterology
2005;128:1838-44.
9. Vakil
N, Moayyedi P, Fennerty MB, Talley NJ. Limited value of alarm features in the
diagnosis of upper gastrointestinal malignancy: systematic review and
meta-analysis. Gastroenterology 2006;131:390-401; quiz 659-60.
10. Moayyedi
P, Soo S, Deeks J, Delaney B, Harris A, Innes M, Oakes R, Wilson S, Roalfe A,
Bennett C, Forman D. Eradication of Helicobacter pylori for non-ulcer
dyspepsia. Cochrane Database Syst Rev 2006:CD002096.
11. Moayyedi
P, Soo S, Deeks J, Delaney B, Innes M, Forman D. Pharmacological interventions
for non-ulcer dyspepsia. Cochrane Database Syst Rev 2006:CD001960.
12. Tack
J, Bisschops R, Sarnelli G. Pathophysiology and treatment of functional
dyspepsia. Gastroenterology 2004;127:1239-55.
13. Soo
S, Moayyedi P, Deeks J, Delaney B, Lewis M, Forman D. Psychological
interventions for non-ulcer dyspepsia. Cochrane Database Syst Rev
2005:CD002301.